A safer way to biopsy the prostate
/A/Prof Grummet was invited to write this article as a guest blog on Adelaide Urologist Dr Nicholas Brook’s website in February 2014.
What's wrong with the current standard method of prostate biopsy?
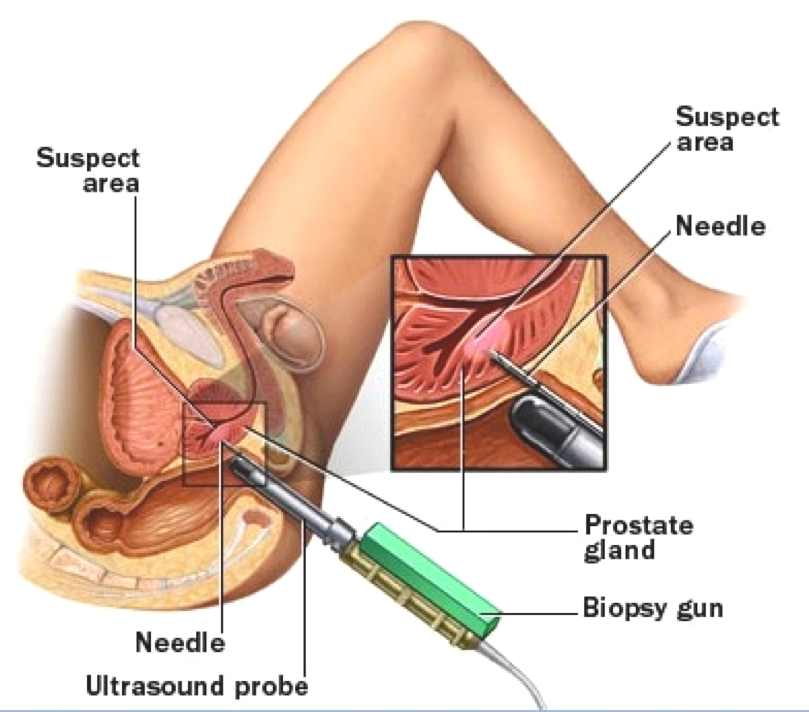
A biopsy is where a sample of tissue is taken for examination under a microscope, usually to determine if cancer is present. As you can see from the diagram below, the easiest way to access the prostate is via the rectum. That’s why we perform a rectal examination - so we can feel the back of the prostate for any suspicious lumps. Most prostate cancers are located towards the back of the prostate (peripheral zone), so a transrectal ultrasound-guided (TRUS) biopsy is a convenient way of sampling this area. Typically, at least 12 cores of tissue are taken during a TRUS biopsy.
The other advantage of the TRUS biopsy is that it can be performed in just a few minutes by giving the patient intravenous sedation or using a local anaesthetic nerve block.
However, passing the needle of the biopsy gun through the wall of the rectum multiple times is problematic. As you’d expect from an organ that stores faeces, the rectum has a high concentration of bacteria. These bacteria don’t cause any problems as long as they stay in the rectum. However, passing the biopsy needle through the wall of the rectum allows these bacteria to access the prostate and its rich blood supply. This in turn can lead to a serious infection in the blood called septicaemia (sepsis). Septicaemia makes patients feel very unwell, requires hospitalization for intravenous antibiotic therapy, and can even be life-threatening.
This risk of sepsis in TRUS biopsy is well-recognised. It is therefore standard to use an antibiotic to help prevent such an infection. Unfortunately, the antibiotic doesn’t always work, so there is still a risk of sepsis, which has been measured at about 2% in Victoria.
Today, there is the additional and growing problem of bacteria developing antibiotic resistance. This has been reported worldwide and was the subject of a major US Government report last year.
Our own research group, the Victorian Transperineal Biopsy Collaboration (VTBC), reviewed the scientific literature, finding that developing resistance is a particular problem for bacteria that live in the rectum, so that the antibiotics we would normally use, such as ciprofloxacin, can sometimes be rendered ineffective. This coincides with reports of increasing rates of TRUS biopsy sepsis, even as high as 5%.
Our research has also found that, as a result of the above, some Australian and New Zealand urology practices have resorted to using big-gun broad-spectrum antibiotics on a regular basis to prevent TRUS biopsy sepsis. Whilst this may reduce sepsis for the individual patient, from a public health perspective, it is a step backwards, as widespread use of such antibiotics will lead to even more resistance. Unfortunately, we are already seeing this happening, with hospitals in Australia finding CRE (Carbapenem-Resistant Enterococci) in their wards.
What is transperineal biopsy, and why is it safer?
Fortunately, there is another approach to prostate biopsy which avoids perforation of the rectum altogether. Instead, the biopsy needle can be passed via the skin of the perineum. In men, the perineum is the part of the body between the scrotum and the anus.
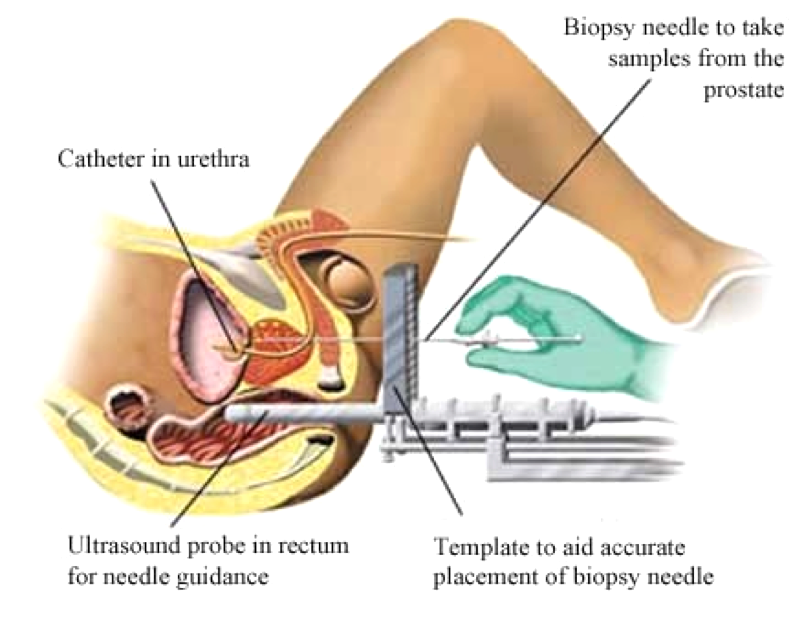
As shown in the diagram, the ultrasound probe is still passed into the rectum to provide an image of the prostate. But instead of the biopsy needle passing alongside the probe, it is passed through a grid, which itself is fixed against the probe outside the body. Prior to insertion of the ultrasound probe, the perineal skin is easily prepared in a sterile fashion, just as any other incision site is prepared before surgery to prevent wound infection. (Although worthwhile attempts have been made to sterilize the rectum, this has not been possible.)
Our group studied the experience of transperineal (TP) biopsy around the world and found that in over 6,600 patients, there were only 10 patients re-admitted to hospital for sepsis - a rate of just 0.076%, or less than 1 in a thousand. Furthermore, in our own published experience of 245 TP biopsies, our rate of re-admission for infection was zero. (We have now performed over 450 TP biopsies, still without a single episode of infection.)
See the abstract of our paper here >
Based on the published scientific evidence to date then, it appears that TP biopsy is a safer option than TRUS biopsy due to its near-zero sepsis risk. It also gives the advantage of avoiding regular use of heavy-duty antibiotics, thereby avoiding promotion of resistant bacteria, now labelled by the US Government Center for Disease Control as a Serious Threat to population health worldwide. As a result, we now use TP biopsy routinely for all prostate biopsies.
Are there any downsides to the transperineal approach?
Looking at the diagram above, you would expect TP biopsy to be painful, which is why it is typically performed under a general anaesthetic (although methods of using local anaesthetic only have been reported). We routinely perform TP biopsy under GA. As a result, men experience no pain during the procedure, and very little afterwards, so that paracetamol is only required occasionally. Although a general anaesthetic is required, it is of a short duration only (less than 30 minutes) and is very safe.
Practitioners of TP biopsy initially reported a higher risk of acute urinary retention (unable to pass urine) with this approach. However, with further experience, and by deliberately avoiding the area around the urethra, this rate dropped so that it is now similar to the risk seen in TRUS biopsy (around 3%). Although a catheter has been used by some doctors, as shown in the diagram above, it is unnecessary.
Due to anecdotal experience, some urologists have been concerned that TP biopsy may lead to erectile dysfunction by damaging the erectile nerves or to more difficult surgery if cancer is found and the prostate needs to be removed. However, evidence to date, albeit scant, does not support either of these concerns.
Is it as good as TRUS at cancer detection?
According to the scientific literature, TP biopsy is at least equivalent to TRUS biopsy in its ability to detect cancer. Some research has also found improved detection of cancers at the front of the prostate (anterior). This may be due to the typically easy access TP biopsy provides to all areas of the prostate, particularly anteriorly. Conversely, it can often be difficult to reach the anterior prostate via TRUS biopsy, especially in large glands.
What other advantage might TP biopsy provide?
In TP biopsy, the ultrasound probe is stabilized by equipment that is fixed to the operating table. The grid through which the biopsy needle is passed is, in turn, stabilized against the ultrasound probe. This set-up permits accurate and reproducible biopsy needle placement.
In the past, TP biopsies were taken in a systematic fashion only, evenly sampling various areas of the prostate. Whilst this is still performed routinely, in addition we are now regularly performing targeted biopsies of suspicious lesions if found on a prostate MRI. The stable arrangement of TP biopsy therefore permits accurate targeting of such lesions, with the potential to further improve the accuracy of cancer detection.